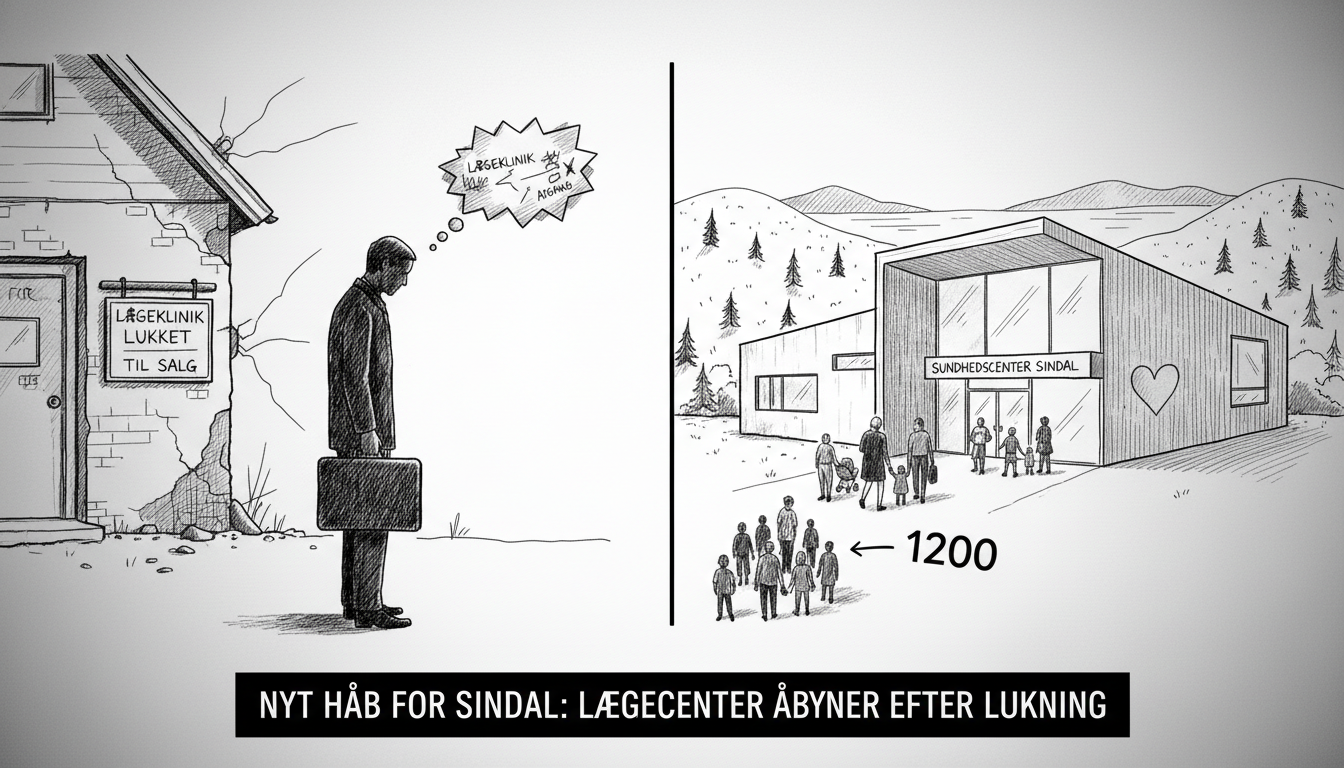
A new medical practice will open in Sindal, Denmark, bringing relief to 1,200 patients left without local healthcare services. The development follows the closure of clinics operated by doctor Morten Krause Nielsen in both Sindal and Sæby.
The doctor faced substantial professional criticism earlier this year regarding multiple patient cases. The scrutiny emerged prominently in a television documentary that examined his medical practice. Regional health authorities subsequently removed his patients from his care.
Patients from Sindal received offers to transfer to a regional clinic in Frederikshavn. The existing second medical practice in Sindal lacked capacity to accommodate the large number of displaced patients. This situation created healthcare access challenges for the local community.
The new medical center will operate from a former kindergarten building in Sindal. This location provides appropriate facilities for medical services and offers convenient access for community members. The conversion represents a practical solution to the town's healthcare gap.
Denmark's healthcare system operates through a combination of public hospitals and privately practicing physicians who contract with regional health authorities. When a general practitioner loses their authorization or closes their practice, the regional health authority must ensure continuity of care for affected patients.
This situation highlights the vulnerability of rural healthcare infrastructure in Denmark. Smaller communities like Sindal often depend on individual practitioners. When one departs, the entire local healthcare system faces disruption. The regional health authority's intervention demonstrates the system's safety net function.
The documentary that brought attention to the doctor's practice raised broader questions about healthcare quality oversight. Medical authorities face the challenge of balancing practitioner autonomy with patient protection. This case shows how media scrutiny can trigger regulatory action.
For international readers, this story illustrates Denmark's decentralized healthcare model. The country divides healthcare responsibility among five regions that manage hospitals and contract with general practitioners. This structure differs significantly from both fully socialized systems and insurance-based models.
The new medical practice's establishment will restore essential services to Sindal residents. Patients will no longer need to travel to neighboring municipalities for routine medical care. The solution addresses both practical healthcare needs and community concerns about local service availability.
What does this mean for healthcare in smaller Danish communities? It demonstrates both the fragility and resilience of rural medical services. While the departure of a single practitioner can create crisis, the system contains mechanisms for recovery. The speed of this response suggests regional authorities prioritized resolving the situation.
The incoming medical practice will likely face heightened scrutiny from both patients and regulators. Community members will understandably approach the new arrangement with caution given recent experiences. Building trust may require transparent communication and demonstrated commitment to quality care.
This development represents positive news for North Jutland residents who depend on accessible local healthcare. The resolution came relatively quickly compared to similar situations in other rural areas. The outcome suggests lessons were learned from previous healthcare transitions in Denmark's smaller communities.