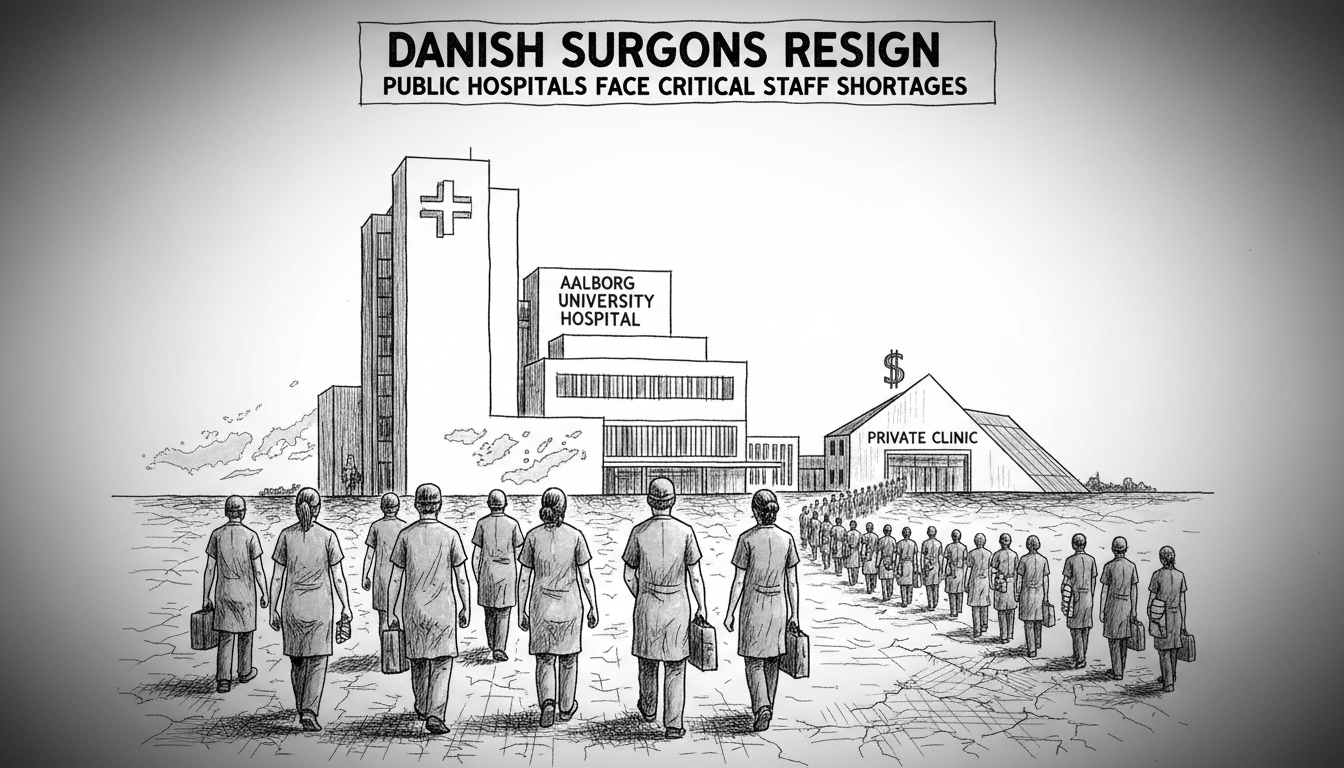
Patients needing hand surgery in Northern Denmark now face dramatically extended waiting times. The orthopedic surgery department at Aalborg University Hospital struggles with severe doctor shortages. Ten experienced surgeons have resigned from the department within the past eighteen months. This staffing crisis reflects broader challenges within Danish society news and the welfare system.
Regional authorities now pay private hospitals to perform public healthcare procedures. This temporary solution addresses immediate patient needs but raises questions about Denmark's social policy direction. The Danish welfare system traditionally provides universal healthcare through public institutions. Current pressures test this model's resilience.
Why do skilled surgeons leave public hospitals? Multiple factors contribute to this exodus. Workload pressures, administrative burdens, and compensation disparities all play roles. These departures affect specialized care availability across Danish municipalities. Copenhagen integration challenges sometimes differ from regional realities, yet both face healthcare workforce issues.
Healthcare professionals express concern about long-term consequences. One medical leader noted the difficulty maintaining surgical training programs with reduced senior staff. Another official described the situation as unsustainable for both patients and remaining healthcare workers. Denmark immigration policy could potentially help address medical workforce gaps, though integration of foreign-trained doctors presents its own challenges.
Historical context shows Denmark previously maintained shorter medical wait times than many European counterparts. Recent statistics indicate waiting periods for certain procedures have doubled in some regions. Educational pipelines for medical specialists require seven to ten years of training after medical school. This lengthy preparation period makes quick solutions difficult.
International readers might wonder how this affects Denmark's renowned quality of life. Healthcare accessibility remains central to the Danish social contract. Current strains could influence public debate about welfare system funding and structure. Regional differences in service availability may also prompt discussions about equitable resource distribution.
What comes next for Danish healthcare? Regional health authorities continue developing both short-term and long-term strategies. These include recruitment initiatives, workload management improvements, and potential structural reforms. The situation in Northern Denmark offers important lessons for healthcare planning nationwide. Other Scandinavian countries monitor these developments closely as they face similar demographic and workforce challenges.
The fundamental question remains how Denmark will preserve its comprehensive healthcare model while adapting to contemporary realities. This involves balancing immediate patient needs with sustainable long-term solutions. The answers will shape Danish society for years to come.