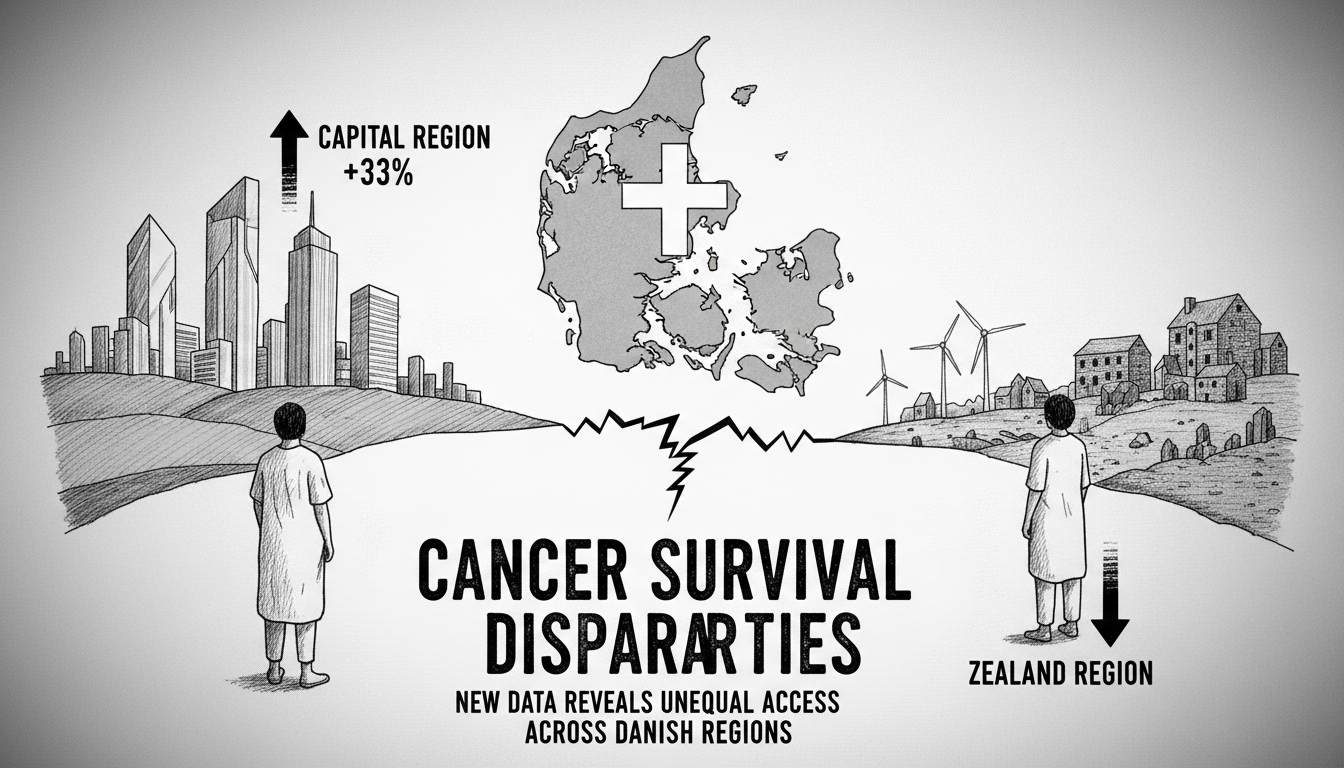
Cancer patients face dramatically different survival odds depending on where they live in Denmark. New figures reveal a troubling healthcare gap between regions that determines life and death outcomes.
Recent data from the Danish Lung Cancer Group shows lung cancer patients in the Capital Region enjoy a 33 percent higher five-year survival rate than those in Zealand Region. For every 100 patients diagnosed, eight more people remain alive after five years in the capital compared to Zealand.
Medical professionals express deep concern about these geographic inequalities. Torben Riis Rasmussen, chief physician and chairman of the Danish Lung Cancer Group, stated bluntly about the situation. He said the disparities are unacceptable and that healthcare equality must be guaranteed for all citizens.
The numbers speak volumes. Only 22.8 percent of lung cancer patients in Zealand Region survive five years post-diagnosis. Meanwhile, the Capital Region achieves a 30.4 percent survival rate. This pattern isn't limited to lung cancer. Previous research examining overall cancer survival rates from 2007 to 2021 showed Zealand consistently ranking lowest nationwide.
Helle Skov from Hørve in Zealand Region received her lung cancer diagnosis one year ago. She described the moment as one of life's worst shocks. Since her diagnosis, she has endured a chaotic treatment journey across multiple hospitals in Næstved, Odense, Holbæk, Roskilde, and Køge. She has encountered 10 to 12 different doctors with varying approaches at each location.
Medical investigators examined whether poorer hospital treatment caused the survival gap. Their research couldn't confirm this theory. Instead, evidence suggests patients in Zealand seek medical help later and receive delayed diagnoses. By the time treatment begins, the disease has often progressed further.
The healthcare access problems in Zealand Region are structural and systemic. The region has only 3.8 doctors per 1,000 residents. The Capital Region boasts 5.7 physicians per 1,000 people. This doctor shortage creates tangible barriers for patients. Helle Skov notes the impossibility of getting timely appointments. The entire process happens over the phone if you can get through at all.
Regional Council Chair Trine Birk Andersen acknowledges the problem. She admits the healthcare system has developed unevenly. Many citizens find it difficult to navigate, and staffing shortages persist. The region competes fiercely with the Capital Region to recruit new doctors but struggles to match its neighbor's appeal.
These health outcome disparities directly influenced national healthcare reform. Parliament decided to merge Zealand and Capital regions partly to address these inequalities. The new Eastern Denmark Region aims to create more uniform healthcare standards.
Medical experts voice caution about the merger solution. Combining regions with good and poor survival rates creates statistical averages that might mask underlying problems. Continuous monitoring of former regional performance remains essential.
For patients like Helle Skov, the healthcare journey continues despite initial successful treatment. Her cancer has returned, this time in lymph nodes. She lives with the anxiety of wondering whether she'll be among those who don't survive five years or whether she'll get to continue living a good life.
The situation highlights critical challenges in Denmark's universal healthcare system. Geographic disparities in cancer survival rates raise questions about equal access to quality care. As healthcare reforms proceed, patients and doctors alike watch closely to see if merger solutions can truly bridge the survival gap between regions.